Final Practical long case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box"
35 year old male came to our hospital on 1/02/2022 with chief complaints of upper abdomen pain since one week,fever since one week ,backpain since 4 days.
Patient was apparently asymptomatic 20 days back ,then he observed yellowish discolouration of eyes and got admitted to near by hospital,later 1week back he developed pain abdomen which was insidious in onset, gradually progressive. Pain in right hypochondrium and gastric region which is aggrevated on sleeping during night and relieved during standing,4 days back he developed back pain ,which is dull aching type.
Fever is on and off since one week, high grade not associated with chills and rigor, cold, cough, body pains.
No history of nausea , vomiting,loose stools.
No history of bleeding manifestations.
No history of renal stones
PAST HISTORY
Not a k/c/o DM,HTN,asthma , epilepsy,TB .Had a hernia operation 8 years back
PERSONAL HISTORY
Diet - mixed
Appetite - decreased since 1 week
Sleep- adequate
Bowel movements- dark stools
Bladder -yellow urine with burning sensation
Addictions- alcohol,360 ml, regular, since 10 years
Smoking -20 cigarettes per day since 10years
General physical examination
Pt is conscious, coherent, cooperative,well oriented with place and person.
No sign of clubbing, cyanosis
Icterus- present
Bipedal edema present
Vitals-
Temp- afebrile
Bp-110/70 mm hg
Pr- 86 bpm
Rr-20 cpm
Spo2- 98% on RA
Systemic examination
RS- bae+
Cvs-S1 S2 +
P/A - tenderness + at right hypochondrium and epigastric region
Cns- nad
Investigations
3/2/22
HB-10.2
TLC- 17,900
PLT- 5.1
Serum amylase- 60
Serum lipase- 28
RFT
Serum urea- 37
Serum creatinine- 1.1
Sodium- 130
Potassium- 6
Chloride- 98
3/2/22
LFT
TB- 4.40
DB- 3.12
AST/ALT- 96/145
ALP- 586
TP- 5.3
Alb- 2.6
A/G- 0.94
PT -17 sec
APTT- 34 sec
INR- 1.25
Diagnosis
Liver abscess secondary to ? Amoebic or pyogenic
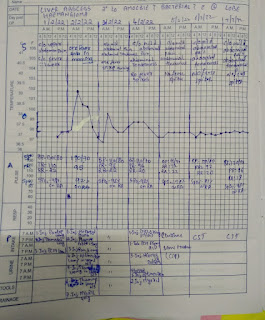
Clinical images
Plan of treatment
1. INJ. METROGYL 750MG/IV/TID
2. INJ. MAGNEX FORTE 1.5MG/IV/BD
3. INJ. PAN 40MG/IV/BD
4. INJ. THIAMINE1 AMP IN 100ML NS/IV/ OD OVER 30 MIN
5. INJ. TRAMADOL 1 AMP IN 100ML NS/IV/OVER 30MIN/ SOS
6. INJ. DICLOFENAC 3ML=75MG IM/BD
7. TAB. PCM 650 MG PO/QID
8. INJ. NEOMOL 1G IV/sos










Comments
Post a Comment